Millard-Gubler syndrome
OVERVIEW
What is Millard-Gubler Syndrome?
"Millard-Gubler Syndrome" is a classic "brainstem syndrome" (a collective term for several brainstem disorders) caused by unilateral pontine lesions, often involving (i.e., invading or damaging) the abducens nerve, facial nerve, pyramidal tract, spinothalamic tract, and medial lemniscus.
French physicians Auguste Louis Jules Millard and Adolphe-Marie Gubler first described its clinical features in 1858, hence the name "Millard-Gubler Syndrome."
Is Millard-Gubler Syndrome Serious?
Yes.
Even with mild symptoms, "Millard-Gubler Syndrome" can severely impact daily life. In severe cases, it not only has a high mortality rate but also imposes a significant burden on patients and their families.
SYMPTOMS
What are the manifestations of Millard-Gubler syndrome?
The typical manifestations of "Millard-Gubler syndrome" include:
-
Impaired abduction of the affected eye:
Due to paralysis of the lateral rectus muscle, one eye cannot move outward, causing diplopia (double vision).
-
Peripheral facial palsy on the affected side:
The facial muscles on the affected side become slack, with loss of forehead wrinkles, flattening of the nasolabial fold, and deviation of the mouth.
-
Contralateral limb hemiplegia (excluding the face):
Inability to move the upper and lower limbs on the opposite side (e.g., paralysis of the left arm and leg if the lesion is on the right), accompanied by impaired deep and superficial sensations (position sense, motion sense, vibration sense, temperature sense, pain sense, and touch sense). This occurs on the opposite side of the facial palsy (e.g., left facial palsy with right limb hemiplegia).
Where does Millard-Gubler syndrome commonly occur?
"Millard-Gubler syndrome" occurs in the ventrolateral part of the "pons," primarily involving the abducens nerve, facial nerve, pyramidal tract, spinothalamic tract, and medial lemniscus.
Among these, damage to the abducens nerve (invasion or impairment, same below) on one side causes ipsilateral esotropia (inward eye deviation), damage to the facial nerve leads to ipsilateral peripheral facial palsy, and damage to the pyramidal tract results in contralateral limb hemiplegia.
What conditions should Millard-Gubler syndrome be differentiated from?
"Millard-Gubler syndrome" needs to be differentiated from other brainstem syndromes:
-
Foville syndrome:
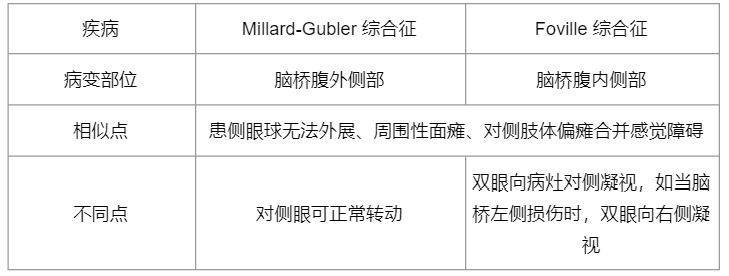
-
Raymond-Cestan syndrome:
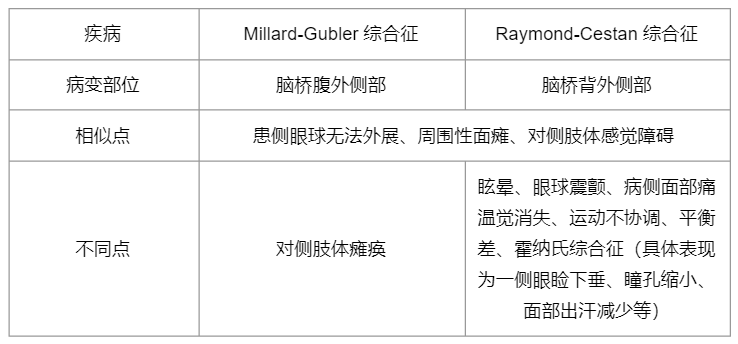
When the lesion is extensive, "Millard-Gubler syndrome" may coexist with the above conditions. Therefore, these distinctions are for reference only, and definitive diagnosis and treatment still require imaging to determine the location and extent of the lesion.
CAUSES
What are the causes of Millard-Gubler syndrome?
The common causes vary among patients of different age groups.
For younger patients, common causes include tumors, multiple sclerosis, tuberculous meningitis, neurocysticercosis (a parasitic disease), viral encephalitis, etc.
In elderly patients, the most frequent causes are vascular accidents, such as cerebral hemorrhage and cerebral infarction.
Who is more likely to develop Millard-Gubler syndrome?
Millard-Gubler syndrome has various causes, and there is no clearly defined "high-risk group" (i.e., individuals with a higher probability of developing the condition than the general population).
DIAGNOSIS
How is Millard-Gubler syndrome diagnosed?
- Examine the patient for typical clinical manifestations in the upper and lower limbs, as well as the sixth and seventh cranial nerves (abducens and facial nerves).
- Obtain a detailed medical history to identify the cause and rule out other etiologies.
- Use auxiliary examinations to further determine the lesion location and cause.
What auxiliary tests are needed for Millard-Gubler syndrome?
-
Computed tomography (CT) and magnetic resonance imaging (MRI):
Helpful in detecting lesions. In addition to cerebral infarction and hemorrhage, conditions such as tuberculomas, tumors, and parasitic diseases can also be identified through imaging.
-
Angiography:
If the injury is caused by vertebrobasilar artery occlusion, angiography can help identify the responsible vessel.
-
Other tests:
For example, a complete blood count can help assess for infection, tumor markers may reveal potential tumors, and cerebrospinal fluid tests aid in ruling out causes.
TREATMENT
Which department should I visit for Millard-Gubler syndrome?
Neurology, Neurosurgery.
Can Millard-Gubler syndrome heal on its own?
No.
Patients should seek medical attention as soon as possible, as early treatment aids in recovery.
Does Millard-Gubler syndrome require hospitalization?
Yes.
How is Millard-Gubler syndrome treated?
Treatment primarily depends on the cause of Millard-Gubler syndrome. Addressing the underlying condition is essential to prevent further nerve damage. Examples of targeted treatments include:
- For patients with "cerebral infarction" as the cause: Early intravenous thrombolysis or endovascular intervention.
- For patients with "tumors" as the cause: Radiation or chemotherapy. Surgical removal may be considered if feasible, but pontine tumors remain a global medical challenge with poor prognosis.
- For patients with "nervous system infections" as the cause: Targeted anti-infective therapy.
Does Millard-Gubler syndrome require rehabilitation?
Yes.
Millard-Gubler syndrome involves hemiplegia, and rehabilitation exercises help restore function.
Common rehabilitation therapies include electrical stimulation, physical therapy, and occupational therapy, which assist patients in improving function and adapting to daily life.
DIET & LIFESTYLE
Can patients with Millard-Gubler syndrome fully recover?
It depends on the severity of neurological deficits, the patient's age, comorbidities (other diseases coexisting with the primary condition), and the underlying cause.
Patients with smaller lesions tend to have milder symptoms and usually have a better prognosis. In contrast, cases involving extensive damage or caused by pontine tumors often have a poorer prognosis due to limited treatment options.
What should Millard-Gubler syndrome patients pay attention to in daily life?
The following points should be noted:
-
Strive to adapt to and overcome sensory impairments.
After treatment, patients may still experience double vision and sensory disturbances, requiring time to adjust to changes in spatial awareness and sensation.
-
Adhere to rehabilitation exercises.
Patients should consult professional doctors to choose appropriate rehabilitation methods, avoiding overexertion that may worsen symptoms. Scientific rehabilitation exercises aid functional recovery and daily adaptation.
-
Maintain personal hygiene.
Patients should develop and maintain good hygiene habits, but limited mobility makes this challenging. Family members can provide assistance.
-
Wear suitable clothing.
Choose easy-to-wear clothing. Buttons and shoelaces can be troublesome for those with hemiplegia—family assistance may be necessary.
-
Prevent strokes.
Patients should improve lifestyle habits, control blood pressure, blood sugar, and cholesterol, quit smoking, lose weight, exercise moderately, and take antiplatelet or anticoagulant medications as prescribed.
What should family members of Millard-Gubler syndrome patients do?
-
Provide emotional support.
Encourage and help patients gradually accept and adapt to physical and lifestyle changes, sharing their psychological burden. Seek help from a psychologist if needed.
-
Supervise and assist with rehabilitation exercises.
Help patients perform appropriate exercises to restore physical function and adapt to daily life.
-
Adjust the patient's diet.
If hemiplegia affects the dominant side, patients may struggle with fine motor skills needed for eating. Family members can offer easy-to-eat foods and use spoons instead of chopsticks or forks.
-
Assist with personal hygiene.
Due to mobility limitations, family members should help maintain hygiene, which aids recovery and boosts the patient's confidence.
PREVENTION
How to Prevent Millard-Gubler Syndrome?
There are many causes of "Millard-Gubler syndrome," and there are no clear preventive measures.
However, individuals can maintain good lifestyle habits in daily life, such as regular physical exercise and a healthy diet, to reduce the risk of cardiovascular diseases.