Osteoarthritis
OVERVIEW
What is osteoarthritis?
Osteoarthritis is a common chronic disease and a degenerative joint disorder caused by various factors such as aging, obesity, overuse, trauma, congenital joint abnormalities, and joint deformities. It manifests as the degeneration and damage of articular cartilage, bone spurs at the joint margins and subchondral bone, leading to clinical symptoms such as joint pain, stiffness, deformity, and functional impairment [1].
In the early stages, the main treatments include weight loss, rest, strengthening muscle strength, using walking aids or crutches, and wearing knee braces to slow disease progression. For patients who do not respond to conservative treatments, total joint replacement surgery may be required for a complete cure.
Is osteoarthritis the same as bone spurs?
No, they are different. Osteoarthritis is a disease, while bone spurs are merely a phenomenon. Patients with osteoarthritis may develop bone spurs.
Bone spurs can occur in almost any bone in the body. When they develop in joints and cause clinical symptoms, they are considered a manifestation of osteoarthritis. In some cases of osteoarthritis, X-rays may show "spurs" on the bones, commonly referred to as "bone spurs" [2].
Is osteoarthritis common?
Yes, it is common. According to reports, there are over 300 million osteoarthritis patients worldwide. In China, the prevalence of primary osteoarthritis (not secondary to other diseases) in people aged 40 and above is as high as 46.3%, meaning approximately 463 out of every 1,000 individuals over 40 have primary osteoarthritis. Moreover, with the increasing aging population in China, the prevalence is gradually rising [3].
Which department should osteoarthritis patients visit for treatment?
Orthopedics or joint surgery.
SYMPTOMS
What are the symptoms of osteoarthritis?
- Pain: The main symptom is joint pain, which is mild and not severe in the early stages but gradually worsens over time. It often occurs in the morning and may lessen after activity, but excessive activity can aggravate it. In advanced stages, persistent pain or nighttime pain may occur.
- Stiffness: Another symptom is joint stiffness, commonly experienced upon waking in the morning or after maintaining a certain posture for an extended period. It usually lasts from a few minutes to over ten minutes and rarely exceeds 30 minutes.
- Other symptoms: Affected joints may also exhibit swelling, tenderness, a grating sensation or "clicking" sounds during movement. In severe cases, muscle atrophy and joint deformities may occur [1].
Which areas are commonly affected by osteoarthritis?
- Knee joint: The most common site. Early symptoms include knee pain when climbing stairs, especially when descending. It may occur unilaterally or alternately on both sides, sometimes accompanied by joint swelling. Severe cases may lead to bow-legged deformity.
- Hip joint: Pain manifests in the outer hip or groin area and may radiate to the knee.
- Finger joints: The interphalangeal joints are most frequently affected, particularly the distal (closer to the fingertips) interphalangeal joints. Swelling, pain, and tenderness are usually mild and rarely impair joint movement. A characteristic feature is the formation of hard nodules due to bony overgrowth on the dorsal sides of the finger joints.
- Spine: Degenerative changes in the vertebrae, intervertebral discs, or facet joints can lead to cervical or lumbar spine issues, causing localized pain and stiffness. In rare severe cases, nerve roots, the spinal cord, or blood vessels may be compressed by bony spurs, resulting in radiating pain or neurological symptoms.
- Foot: The metatarsophalangeal joint of the big toe is the most commonly affected area in the foot. Tight shoes and repeated trauma are contributing factors. Symptoms include localized pain, joint deformity, and hallux valgus (bunions) [4].
Why is osteoarthritis more common in the knee joint?
With age, joint cartilage degenerates and becomes more prone to wear. The greater the load on a joint, the more severe the cartilage wear, increasing the likelihood of osteoarthritis. Therefore, osteoarthritis often occurs in weight-bearing joints.
During walking, the knee joint bears up to four times the body's weight, and this load increases to seven times when climbing stairs or inclines. This makes the knee the most common site for osteoarthritis [4].
Can osteoarthritis cause disability?
Osteoarthritis generally does not lead to disability. A small percentage of patients remain asymptomatic throughout their lives. Most experience joint-related symptoms, such as migratory joint pain (where pain shifts between joints, e.g., starting in the left shoulder and later appearing in the right). In rare cases, nerve compression may cause limb radicular pain or sensory abnormalities [4].
Most patients with neurological symptoms recover after rest or treatment, with only a few developing neurogenic paralysis (e.g., quadriplegia, hemiplegia, or facial paralysis due to spinal cord compression or injury).
Occasionally, osteoarthritis may cause localized joint destruction, leading to functional impairment and deformity.
Do all osteoarthritis patients experience joint pain?
Most osteoarthritis cases develop insidiously and chronically. Over half of patients show no symptoms in the early stages. Some patients exhibit significant bone spurs on X-rays for 10–20 years without pain, while others with mild or no X-ray abnormalities may have severe symptoms. Thus, clinical symptoms do not always align with X-ray findings [4].
Many asymptomatic patients may suddenly develop symptoms due to triggers like fatigue, stress, joint sprains, trauma, fever, cold exposure, or cold water contact, resulting in pain, tenderness, or swelling in one or more joints. Symptoms often resolve quickly with anti-inflammatory medication or physical therapy after addressing the trigger.
CAUSES
What are the types of osteoarthritis and their causes?
Based on the presence or absence of local and systemic pathogenic factors, osteoarthritis is divided into two main categories: primary and secondary:
- Primary osteoarthritis: The exact cause is unclear, and its development is a long-term, chronic, and gradual process. It may be related to factors such as age, obesity, gender, and genetics.
- Age: The incidence increases significantly with age. Studies show that this condition is uncommon in people under 40 but more prevalent in those over 60. This may be due to increased joint wear and bone loss with aging, leading to osteoarthritis.
- Obesity: Overweight individuals experience doubled pressure on their knees while walking, accelerating degenerative joint changes. Obesity is a major risk factor for knee and hip osteoarthritis.
- Gender: Studies indicate a higher incidence in women, especially postmenopausal women, though the exact reason remains unclear. This may be related to estrogen receptors in joint cartilage [1].
- Genetics: There is a genetic predisposition, though the likelihood varies by joint. For example, hand and hip osteoarthritis have a stronger genetic link, while knee osteoarthritis has a weaker one [4].
- Secondary osteoarthritis: This type results from structural changes that cause cartilage degeneration and joint dysfunction, developing due to other conditions such as trauma, inflammation, metabolic disorders, or congenital joint abnormalities [1].
With advances in medicine and deeper research into joint diseases, many cases previously considered primary osteoarthritis have been found to be secondary to other conditions.
Who is prone to osteoarthritis?
Osteoarthritis is common in middle-aged and elderly individuals, with the risk increasing with age. However, it is also closely related to body type, physiological characteristics, and occupational or lifestyle factors. High-risk groups include:
- Age: Higher incidence in the elderly, with prevalence increasing with age.
- Gender: More common in women, especially postmenopausal women.
- Obesity: Obese individuals are more susceptible.
- Ethnic factors: Western populations have higher rates of hip osteoarthritis, while Eastern populations have higher rates of knee osteoarthritis.
- Occupational factors: Certain professions, such as miners, manual laborers, field geologists, athletes, and dancers, are at higher risk due to joint overuse and wear [4].
At what age is osteoarthritis most likely to occur?
Middle-aged and elderly individuals are most susceptible. According to U.S. data, the incidence is 2%–3% in those under 45, 24.5%–30% in those aged 45–64, and as high as 58%–68% in those over 65. In other words, among people under 45, 20–30 per 1,000 have the condition, while among those over 65, 580–680 per 1,000 are affected [2].
Do bone spurs in osteoarthritis develop with age?
Degenerative changes, including bone spurs, occur naturally with aging, especially in weight-bearing or frequently used joints like the neck, lower back, hips, and knees. This is a common physiological phenomenon in middle-aged and elderly individuals, similar to thinning or graying hair, and does not necessarily indicate disease or require treatment.
Treatment is only needed when symptoms such as joint pain, swelling, stiffness, crepitus, or limited mobility appear [1].
Is osteoarthritis hereditary?
Osteoarthritis has a genetic component, meaning if your parents have it, you are more likely to develop it. However, having a family history does not guarantee you will get it—only that your risk is higher than average [4].
DIAGNOSIS
How is osteoarthritis diagnosed?
Diagnosis of osteoarthritis is relatively straightforward based on chronic medical history, clinical manifestations, and X-ray findings. If necessary, synovial fluid analysis can be performed to confirm the diagnosis.
However, since X-ray changes cannot determine whether it is primary osteoarthritis, doctors need to clarify from the medical history whether the lesion is primary or secondary.
What tests are commonly needed for osteoarthritis?
Osteoarthritis is usually diagnosed based on the patient's complaints and the doctor's physical examination, but sometimes additional tests are required. Common tests include:
- Blood tests and inflammatory markers: For patients with fever and polyarthralgia, blood tests, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are usually performed to exclude rheumatic, rheumatoid arthritis, and infectious arthritis. Blood tests in osteoarthritis patients show no abnormalities, but those with acute synovitis may exhibit mild elevations in CRP and ESR [1].
- X-rays: Joint X-rays can reveal gross abnormalities, reflecting the extent of joint damage and disease progression, and are routine tests for osteoarthritis patients.
- CT scans: CT scans offer high resolution, clearly displaying soft tissues, bones, and joints, and are particularly valuable for diagnosing osteoarthritis in areas not easily visualized by standard X-rays.
- Magnetic resonance imaging (MRI): MRI provides clear images of bones, articular cartilage, menisci, ligaments, synovium, and joint effusions, and doctors may choose this based on clinical needs.
- Synovial fluid analysis: Synovial fluid can reveal hemarthrosis, microorganisms, and urate crystals, providing diagnostic value for traumatic, infectious, and gouty arthritis. For difficult-to-diagnose monoarthritis, joint aspiration for synovial fluid analysis may be necessary.
- Arthroscopy and synovial biopsy: Arthroscopy allows direct visualization of lesions and synovial tissue sampling for pathological examination. It can also be used for treatments like loose body removal or synovectomy. Doctors will decide whether this test is needed based on the condition [2].
What abnormalities are found in laboratory tests for osteoarthritis patients?
- Laboratory tests: Most osteoarthritis patients show no abnormalities in lab tests. However, in cases of joint deformity, widespread osteoarthritis, or acute synovitis, mild increases in ESR (rarely exceeding 40 mm/hour), CRP, and white blood cell count may occur.
- Synovial fluid analysis: Most results are within normal range, though some patients may show mild leukocytosis. Elderly patients may exhibit calcium pyrophosphate and/or apatite crystals.
- Immunological tests: Osteoarthritis patients test negative for rheumatoid factor, antinuclear antibodies, and anti-streptolysin O. Positive results suggest possible coexisting rheumatic or autoimmune diseases, requiring further diagnosis [1].
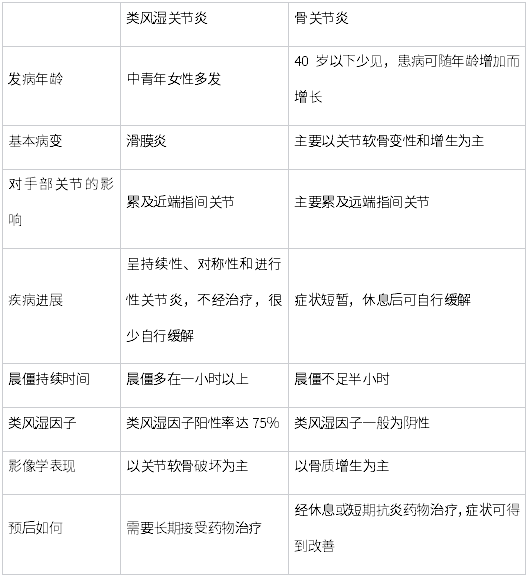
Is osteoarthritis the same as rheumatoid arthritis?
Osteoarthritis and rheumatoid arthritis are both systemic joint diseases that can affect large and small joints, but they are distinct conditions requiring differentiation. Key differences include [1]:
TREATMENT
Can osteoarthritis be completely cured?
Currently, there is no effective medical method to reverse the progression of osteoarthritis. Most patients experience continuous disease progression and worsening, so the vast majority require treatment.
However, conservative treatments cannot completely cure osteoarthritis but can only alleviate symptoms and slow its progression. With early diagnosis, timely treatment, and persistence, the disease progression can generally be controlled, allowing patients to work and live normally.
For patients who do not respond to conservative treatments, total joint replacement surgery is the only definitive solution for osteoarthritis [2].
Does mild osteoarthritis require treatment?
For early-stage osteoarthritis patients with very mild symptoms and no clinical manifestations such as joint pain or stiffness, drug treatment may not be necessary. Instead, physical methods can be used alone, including:
- Weight loss to reduce joint load;
- Balancing work and rest to allow joints adequate rest;
- Engaging in appropriate exercises (avoiding intense activities like running or mountain climbing) such as swimming or cycling;
- Strengthening muscles to share the load on joints;
- Using assistive devices like walkers, canes, or knee braces to redistribute weight.
These physical therapies are the most fundamental treatments and serve as the basis for other approaches.
What are the treatment options for osteoarthritis?
The key to treating osteoarthritis is reducing joint load and excessive movement to delay disease progression. The main treatment methods include:
- Conservative treatment: Weight loss for obese patients to reduce joint load. Using crutches or canes for lower limb joint issues can help alleviate burden. Physical therapy and appropriate exercises maintain joint mobility. Braces or canes may assist in managing acute symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) like acetaminophen or diclofenac can relieve pain [4].
- Surgical treatment: For patients unresponsive to conservative treatments, osteotomy or joint replacement surgery may be considered. Joint replacement is currently the most effective method to eliminate pain, correct deformities, and improve function, significantly enhancing quality of life [1].
What medications are used to treat osteoarthritis?
For early or mid-stage osteoarthritis, drug therapy is simple, effective, and easy to maintain. Common medications include:
- NSAIDs: Such as acetaminophen, diclofenac, or celecoxib, which have anti-inflammatory, analgesic, and antipyretic effects. These are the most commonly used drugs for osteoarthritis and can be purchased over-the-counter.
- Central analgesics: Such as tramadol or opioids. However, due to their addictive nature, opioids require a prescription and must be used under medical supervision [1].
What are the effects of long-term painkiller use for osteoarthritis?
Long-term use of painkillers can cause side effects like liver/kidney damage, gastrointestinal ulcers, or bleeding. The longer and higher the dosage, the greater the risk.
Generally, painkillers are recommended for severe symptoms and should be discontinued after acute pain subsides. Short-term use rarely causes significant side effects [4].
Do osteoarthritis patients need antibiotics?
Osteoarthritis is caused by joint cartilage degeneration, and its "inflammation" is non-infectious (aseptic). Therefore, antibiotics are unnecessary [1].
When is surgery needed for osteoarthritis?
- When loose bodies in the joint affect movement;
- When severe pain persists despite medication;
- When joint instability, severe deformity, dysfunction, or complications occur [2].
What surgical options are available for osteoarthritis?
Common surgeries include arthroscopic debridement, osteotomy, joint fusion, and joint replacement.
- Arthroscopic debridement: Removes cartilage fragments, meniscus debris, or bone spurs, flushing out inflammatory factors. It relieves symptoms but does not halt disease progression.
- Osteotomy: Corrects misalignment (e.g., bowlegs) to redistribute joint load, reduce pain, and delay degeneration.
- Joint replacement: Eliminates pain and restores function, significantly improving quality of life for patients unresponsive to conservative treatments [2-4].
Can intra-articular injections treat osteoarthritis?
Previously, injections were thought to improve joint environment and promote cartilage repair. However, recent studies show limited efficacy, and improper use may worsen symptoms. Caution is advised [3].
What are the pros and cons of steroid injections for osteoarthritis?
While corticosteroids can suppress cartilage degradation and improve symptoms in synovitis cases, long-term use may accelerate cartilage damage. Repeated injections are not recommended [3].
How to treat severe osteoarthritis in young patients?
- Osteotomy: For young patients with severe joint deformity but intact cartilage, osteotomy can correct alignment and delay degeneration.
- Joint fusion: For severely damaged joints, fusion provides stability but sacrifices mobility.
- Joint replacement: Offers mobility but has a limited lifespan (15–20 years). Age is no longer a strict contraindication due to advances in technology [4].
When is joint replacement necessary for osteoarthritis?
For advanced osteoarthritis with severe cartilage degeneration, deformity, and limited mobility, joint replacement is recommended if conservative treatments fail [2].
It significantly improves quality of life for elderly patients and enables younger patients to remain active. Complications like infection or dislocation are rare.
Can joint replacement cure osteoarthritis?
Yes.
Joint replacement is one of the most significant medical advancements of the 20th century, allowing severely affected patients to walk normally and live independently. It is the best solution for end-stage osteoarthritis [2].
What should osteoarthritis patients prepare before surgery?
- Maintain hygiene to reduce infection risk.
- Communicate with healthcare providers and stay positive.
- Practice using a bedpan.
- Control weight and eat a balanced diet (protein, vegetables, fruits). Quit smoking and alcohol.
- Perform pre-surgery exercises (e.g., quadriceps strengthening).
Is physical therapy effective for osteoarthritis?
Physical therapy reduces inflammation, improves blood flow, relaxes muscles, and relieves pain. Early therapy helps maintain joint function and muscle strength.
Common methods include heat therapy, ultrasound, infrared, steam baths, wax therapy, iontophoresis, and massage [1].
Can osteoarthritis recur after treatment?
Osteoarthritis cannot be reversed, and most patients experience progressive worsening. Conservative treatments only alleviate symptoms.
Triggers like weather, stress, or diet can cause flare-ups. Joint replacement is the only definitive solution for refractory cases [1].
Is glucosamine effective for knee osteoarthritis?
Not recommended [5].
While glucosamine was once believed to nourish cartilage, large studies show no significant benefit. Any perceived pain relief may be a placebo effect.
Glucosamine is safe if used as directed but lacks proven efficacy.
What home exercises help osteoarthritis patients?
- Low-intensity exercises like leg lifts, clamshells, bridges, wall squats, and lunges can strengthen muscles and improve balance.
- Water-based exercises (e.g., walking or kicking in a pool) reduce joint load while building strength.
How to rehabilitate after knee replacement surgery?
Rehabilitation starts 3 days post-surgery and continues until full recovery. It is divided into three phases:
- Phase 1 (0–2 weeks): Control pain/swelling, achieve >80° knee flexion, and walk with assistive devices.
- Phase 2 (2–8 weeks): Improve mobility (>105° flexion), correct gait, and climb low steps.
- Phase 3 (8–16 weeks): Restore full function (>115° flexion), strength, and independence.
Avoid overexertion or premature high-impact activities.
DIET & LIFESTYLE
Can bone spurs in osteoarthritis be worn away through exercise?
Bone spurs, also known as osteophytes, are caused by joint degeneration and will not disappear through exercise once they form. Appropriate exercise only helps alleviate symptoms and delay joint degeneration.
Currently, there are no medications that can shrink or remove bone spurs, but inflammation can subside. Reducing inflammation decreases fluid buildup and swelling, thereby relieving pain.
How should osteoarthritis patients engage in physical exercise?
Appropriate physical exercise can improve joint function in osteoarthritis patients.
Exercise should be tailored to the patient's condition, performed within the joint's range of motion, and gradually increased in intensity. Start with non-weight-bearing activities and transition to weight-bearing exercises only after pain subsides.
Recommended exercises include those that improve joint mobility, strengthen surrounding muscles, and enhance endurance, such as walking, cycling, or swimming. These activities increase oxygen capacity, improve cardiovascular function, and regulate glucose and fat metabolism. Severe cases may begin with muscle contractions without joint movement, preferably in water, where body weight is reduced to 1/8 of land weight.
Incorrect exercises, such as those involving excessive joint torque or load (e.g., hiking, stair climbing, or squats), may worsen osteoarthritis and should be avoided.
Is daily hiking or stair climbing beneficial for elderly osteoarthritis patients' knees?
No, it may worsen the condition.
Knee load varies greatly with movement and gait, and excessive load is a risk factor for osteoarthritis. Elderly individuals often struggle to descend mountains because hiking increases joint load four to five times beyond normal levels.
When stairs are unavoidable, osteoarthritis patients should hold railings or walls, avoid taking large steps, and ensure both feet are on the same step before proceeding to reduce joint stress.
What lifestyle and dietary precautions should osteoarthritis patients take?
Since osteoarthritis is linked to obesity, calcium loss, and deficiencies in vitamins A and D, the following precautions are recommended:
- Engage in moderate outdoor activities and avoid prolonged bed rest.
- Consume calcium-rich foods (e.g., milk, eggs, beans, vegetables, and fruits) to meet bone metabolism needs. Elderly individuals require 50% more calcium (≥1200 mg daily), with supplements if necessary.
- Maintain a healthy weight to reduce joint load.
- Limit protein intake, as excess protein promotes calcium loss.
- Increase intake of vitamins A, B1, B6, B12, C, and D.
- Avoid cold, damp environments and direct air conditioning on joints.
Can someone with an artificial metal joint due to osteoarthritis fly after recovery?
Metal implants do not affect air travel. Airline restrictions on metal items are for safety, not health concerns.
After surgery, request a medical note stating "metal implant present" for airport security. Carry this note during flights to avoid inconvenience.
PREVENTION
How to Prevent and Exercise for Osteoarthritis in Daily Life?
- Minimize activities like climbing stairs, hiking, standing for long periods, or lifting heavy objects. High-intensity, long-duration, or weight-bearing activities such as mountain climbing, stair climbing, rock climbing, prolonged walking, or power walking can easily strain the joints and accelerate cartilage wear. These activities should be done in moderation.
- Swimming and walking are joint-friendly exercises that do not increase knee joint load while strengthening the surrounding muscles and ligaments. However, avoid excessive duration—30 minutes to an hour is ideal.
- Reduce joint stress. Maintaining a healthy weight significantly lowers the risk of osteoarthritis, and avoid wearing high heels.
- Keep joints warm and dry to avoid excessive cold or dampness.
- Schedule an annual full-body check-up to detect and address abnormalities early.